PIVD (Prolapsed Intervertebral Disc)
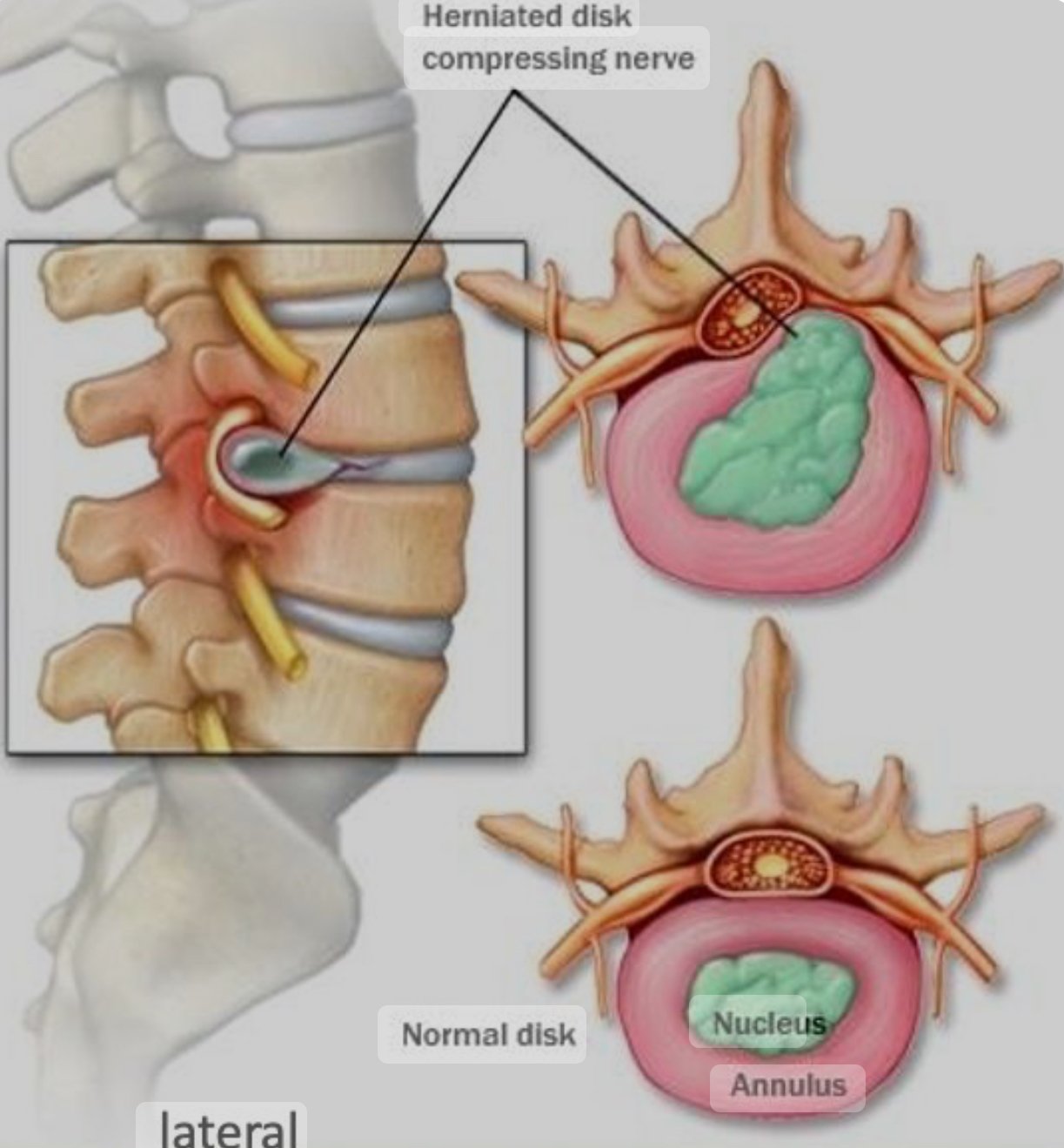
Prolapsed Intervertebral Disc (PIVD), also known as a herniated disc or slipped disc, occurs when the inner gel-like core of a spinal disc (nucleus pulposus) bulges out through a tear in the outer layer (annulus fibrosus). Because it puts pressure on adjacent nerves, this condition may produce discomfort, numbness, or weakness in the affected area.

Mechanisms of PIVD (Prolapsed Intervertebral Disc)
A Prolapsed Intervertebral Disc (PIVD), commonly referred to as a herniated or slipped disc, occurs when the inner gel-like nucleus pulposus protrudes through a tear in the outer fibrous ring (annulus fibrosus) of an intervertebral disc.* This protrusion can compress nearby nerves, leading to pain and other symptoms. The mechanisms leading to PIVD can be broadly categorised into mechanical, biochemical, and degenerative processes.
1. Mechanical Mechanisms
– Disc Loading and Compression:
– Repeated loading and compressive forces on the spine can cause micro-tears in the annulus fibrosus. Over time, these small injuries can accumulate, weakening the outer ring and allowing the nucleus pulposus to protrude .
– Sudden traumatic events, such as heavy lifting with improper technique or a fall, can also cause immediate disc herniation.
– Flexion and Torsion Movements:
– Movements that involve bending forward (flexion) and twisting (torsion) can increase pressure on the discs, particularly in the lumbar spine. These movements can lead to annular tears and subsequent herniation .
2. Degenerative Mechanisms
– Age-Related Degeneration:
– With age, the intervertebral discs lose hydration and elasticity. The nucleus pulposus becomes less gel-like and more fibrous, reducing its ability to evenly distribute pressure. This makes the disc more susceptible to herniation .
– The annulus fibrosus also weakens with age, becoming more prone to tears and fissures.
– Disc Degeneration:
– Degenerative disc disease (DDD) involves the gradual deterioration of the intervertebral discs. This process is characterized by a decrease in disc height, formation of bone spurs (osteophytes), and increased brittleness of the annulus fibrosus【5†source】.
3. Biochemical Mechanisms
– Inflammatory Processes:
– The nucleus pulposus contains pro-inflammatory substances that can induce inflammation when they come into contact with spinal nerves. This inflammation can exacerbate pain and other neurological symptoms associated with PIVD【6†source】.
– Biochemical changes in the disc, such as increased levels of cytokines and matrix metalloproteinases, contribute to disc degradation and inflammation.

4. Risk Factors
– Genetic Predisposition:
– Genetics can play a role in the susceptibility to disc herniation. Individuals with a family history of disc problems may be more likely to experience PIVD .
– Occupational and Lifestyle Factors:
– Jobs that involve repetitive lifting, bending, or prolonged sitting can increase the risk of developing PIVD. Sedentary lifestyles and poor physical conditioning also contribute to the weakening of the supporting musculature around the spine .
– Obesity:
– Excess body weight places additional stress on the intervertebral discs, particularly in the lumbar region, increasing the risk of herniation .
Conclusion
PIVD is the consequence of metabolic processes, degenerative changes, and mechanical forces combined.With the use of ergonomic techniques, focused physiotherapy interventions, and appropriate lifestyle modifications, the condition can be prevented and managed with an understanding of these causes.
The stages of Prolapsed Intervertebral Disc (PIVD) are:
1. Disc Degeneration: The intervertebral disc shows signs of wear and tear, but the disc shape is maintained. It may cause minor pain or discomfort.
2. Prolapse (Protrusion): The nucleus pulposus (inner gel-like core) begins to push through the annulus fibrosus (outer ring), causing a bulge that does not rupture the outer layer. In this stage, it can cause pressure on spinal nerves, leading to pain.

3. Extrusion: The nucleus pulposus breaks through the annulus fibrosus but remains within the disc. In this stage, it can lead to more severe nerve compression and increased pain or neurological symptoms.
4. Sequestration: Fragments of the nucleus pulposus break away from the main disc and can move into the spinal canal.
This stage is the worst and can result in acute nerve impingement, which can cause excruciating pain and perhaps function loss like bowl bladder dysfunction.
Each stage progressively increases the risk of nerve damage and the severity of symptoms. The various treatment choices are determined by the illness’s severity and stage.
Physiotherapy Treatment for PIVD
Physiotherapy is a primary treatment approach for managing PIVD and alleviating its symptoms. The AIM of physiotherapy in treating PIVD include reducing pain, improving mobility, and strengthening the muscles supporting the spine. The treatment usually involves several components:
1. Pain Management:
– Modalities: Use of modalities such as heat or cold therapy, ultrasound, and electrical stimulation (e.g., TENS) to reduce pain and inflammation.
– Manual Therapy: Techniques like soft tissue massage, myofascial release, and gentle spinal mobilizations to relieve pain and improve circulation.
2. Exercise Therapy:
– Core Strengthening: Exercises that strengthen the core muscles to provide better support for the spine. The exercises inclides, like pelvic tilts, bridges, and planks.
– Flexibility Exercises : Stretching exercises can assist lessen stress on the intervertebral discs by increasing the flexibility of the muscles surrounding the spine.
– Specific Exercises: McKenzie exercises are often recommended for disc problems, focusing on extension movements to centralise pain and reduce disc protrusion.
3. Posture and Ergonomics:
– Education on maintaining proper posture during daily activities and ergonomic adjustments to reduce strain on the spine.
4. Activity Modification:
– Guidance on modifying activities and movements that may aggravate symptoms, promoting safe movement patterns and avoiding heavy lifting or twisting motions.
5. Patient Education:
– Teaching patients about the anatomy and mechanics of their condition, strategies for pain management, and the importance of adhering to their exercise program.
Example Exercises
1. Pelvic Tilt:
– Lie on your back with knees bent and feet flat on the floor. Tighten your abdominal muscles to flatten your back against the floor and hold for a few seconds. Repeat several times.

2. Bridging:
– Lie on your back with knees bent and feet flat. Lift your hips towards the ceiling while keeping your shoulders on the ground, forming a bridge with your body. Hold and then lower slowly.
3. McKenzie Extension:
– Lie face down, then prop yourself up on your elbows while keeping your hips on the floor. Hold for a few seconds and repeat, gradually increasing the duration as tolerated.
Additional Considerations
– Consistency: Regular and consistent exercise and adherence to physiotherapy recommendations are crucial for effective management of PIVD.
– Professional Guidance: Always perform exercises under the supervision of a licensed physiotherapist to ensure proper technique and avoid further injury.
– Gradual Progression: Start with gentle exercises and gradually increase intensity as your condition improves and as advised by your physiotherapist.
Physiotherapy plays a critical role in the conservative management of PIVD, aiming to relieve symptoms and improve functional capacity through tailored exercises and therapeutic interventions.
FAQs
Can PIVD cured without surgery ?
Yes, Prolapsed Intervertebral Disc (PIVD) can often be treated and managed without surgery. Non-surgical treatments include:
1. Physical Therapy: Exercises to strengthen the muscles supporting the spine, improve flexibility, and reduce pressure on the disc.
2. Medications: Pain relievers, anti-inflammatory drugs, and muscle relaxants can help manage pain and inflammation.
3. Epidural Steroid Injections: Injections of corticosteroids into the epidural space can reduce inflammation and pain around the affected nerve.
4. Activity Modifications: Avoiding activities that exacerbate symptoms and incorporating rest can help manage pain.
5. Heat and Cold Therapy: Applying heat or cold to the affected area can reduce muscle tension and inflammation.
6. Chiropractic Care: Manual manipulation by a chiropractor can help alleviate pressure on the nerves.
7. Acupuncture: This traditional Chinese medicine technique may help relieve pain.
*Depending on the severity of the ailment and unique patient characteristics, these therapies may or may not be beneficial. Non-surgical treatment often results in significant comfort and better function for individuals
However, if conservative treatments fail to alleviate symptoms, or if there is significant nerve compression leading to severe pain or neurological deficits, surgery may be considered.
Want to know more Please visit the below links:
– [WebMD: Herniated Disc](https://www.webmd.com/back-pain/guide/herniated-disc)
– [Mayo Clinic: Herniated Disc](https://www.mayoclinic.org/diseases-conditions/herniated-disk/symptoms-causes/syc-20354095)
– [Physiopedia: Herniated Disc](https://www.physio-pedia.com/Herniated_Disc)
Read More:
https://physiohealwell.com/2024/06/23/shoulder-dislocation-joint/
https://physiohealwell.com/2024/06/22/foot-pain/
https://physiohealwell.com/2024/06/21/physiotherapy-during-pregnancy/
https://physiohealwell.com/2024/06/21/dha-requirements-in-physiotherapy/