FOOT PAIN
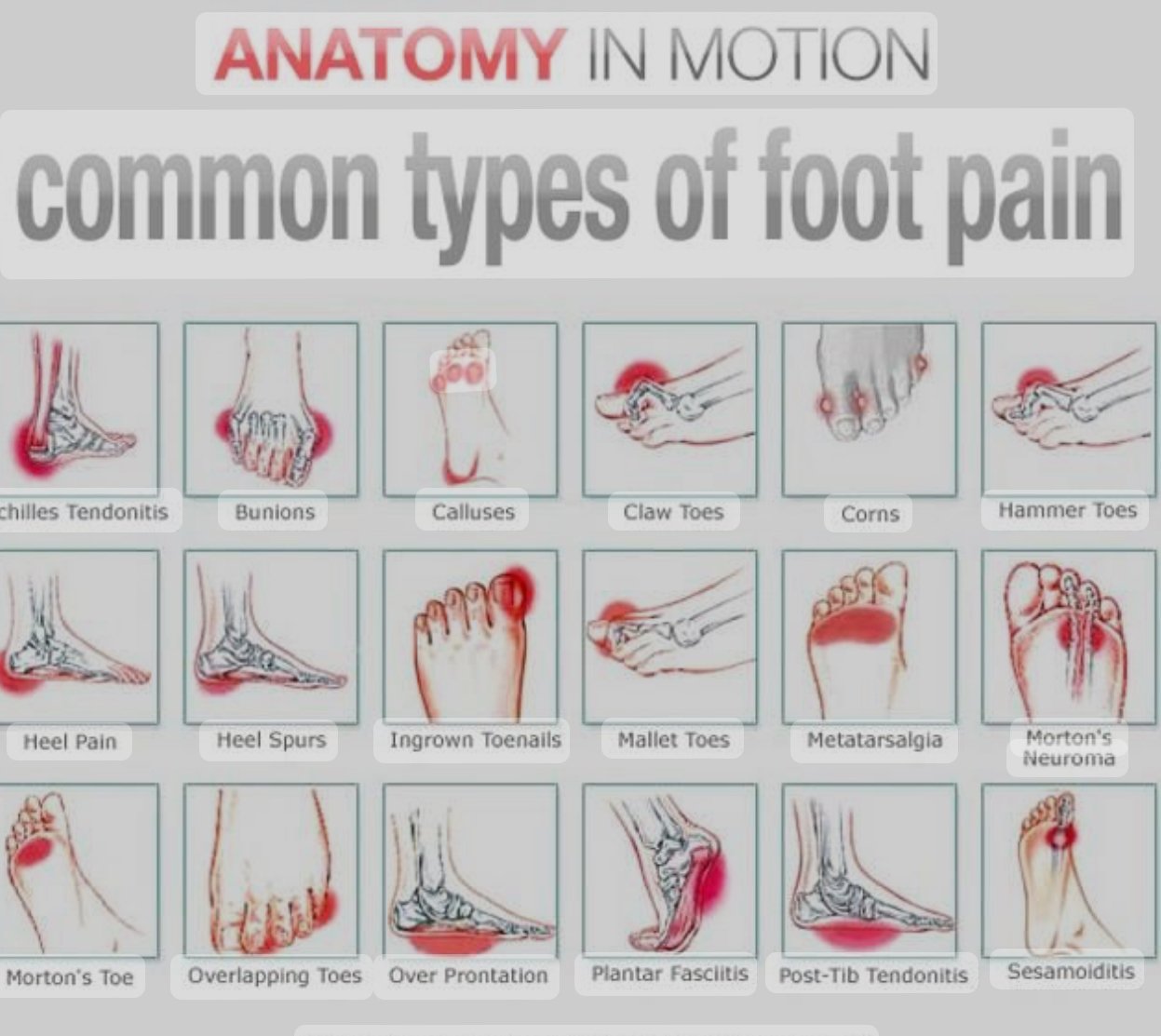
FOOT PAIN can result from a number of ailments and traumas, which are frequently classified according to their location and underlying causes.. Here are some common types of foot pain:
1. Heel Pain
– Plantar Fasciitis: Inflammation of the plantar fascia, causing sharp pain in the heel, especially in the morning.
– Heel Spurs: Calcium deposits causing a bony protrusion on the underside of the heel bone.
– Achilles Tendinitis:Inflammation of the Achilles tendon, causing pain at the back of the heel.
2. Arch Pain
– Flat Feet (Pes Planus): Lack of arch in the foot, leading to strain and discomfort.
– High Arches (Pes Cavus): Excessive arch, causing foot instability and pain.
– Posterior Tibial Tendon Dysfunction: Dysfunction of the tendon supporting the arch, leading to pain and flatfoot.
3. Toe Pain
– Bunions: Bony bumps forming on the joint at the base of the big toe.
– Hammertoes:Abnormal bend in the middle joint of a toe.
– Gout: Arthritis causing severe pain and swelling in the big toe.
4. Ball of Foot Pain (Metatarsalgia)
– Morton’s Neuroma: Thickening of tissue around a nerve leading to the toes, causing sharp pain.
– Stress Fractures: Small cracks in the bones of the foot, often due to overuse.
5. Side of Foot Pain
– Cuboid Syndrome: Dislocation or subluxation of the cuboid bone.
– Perineal: Tendonitis:Inflammation of the peroneal tendons on the outside of the foot.
6. General Foot Pain
– Arthritis: Inflammation of joints, leading to pain, stiffness, and swelling.
– Tendinitis: Inflammation of tendons, commonly in the Achilles or peroneal tendons.
– Neuropathy: Nerve damage, often due to diabetes, leading to pain and numbness.
7. Pain Due to Foot Deformities
– Clubfoot: Birth defect causing the foot to twist inward or downward.
– Charcot Foot: Complication of neuropathy leading to deformity and instability.
8. Pain Due to Infections and Skin Conditions
– Athlete’s Foot:Fungal infection causing itching, burning, and pain.
– Plantar Warts: Hard growths on the bottom of the foot caused by a viral infection.
Depending on the intensity and underlying reason, many therapies are available for different types of foot pain, ranging from rest and physical therapy to medication and surgery. For treatment to be successful, a MEDICAL EXPERT must provide an accurate diagnosis.
Causes of Foot pain
Foot pain can be caused by a various of conditions, Injuries, & Lifestyle factors. Here are some common causes:
1. Injuries:
– Sprains and strains: Overstretching or tearing ligaments and muscles.
– Fractures: Broken bones in the foot.
– Bruises: Trauma to the foot causing bleeding under the skin.
2. Medical Conditions:
– Arthritis: Inflammation of the joints, including osteoarthritis and rheumatoid arthritis.
– Plantar fasciitis: Inflammation of the plantar fascia, a ligament on the bottom of the foot.
– Tendinitis: Inflammation of the tendons, such as Achilles tendinitis.
– Gout: A form of arthritis caused by excess uric acid forming crystals in joints.
– Diabetic neuropathy: Nerve damage due to diabetes, leading to pain and numbness.
3. Structural Issues:
– Flat feet: Lack of arch in the foot can cause pain and fatigue.
– High arches: Excessive arching can lead to strain & pain.
– Bunions: A bony bump forming on the joint at the base of the big toe.
– Hammertoes: Abnormal bend in the middle joint of a toe.
4. Infections:
– Fungal infections: Such as athlete’s foot.
– Bacterial infections: Like cellulitis.
5. Footwear:
– Poorly fitting shoes: Can cause blisters, calluses, and other problems.
– High heels: Can lead to foot pain and deformities.
6. Lifestyle Factors:
– Overuse: Standing, walking, or running for long periods.
– Obesity: Extra weight puts more pressure on the feet.
7. Circulatory Issues:
– Poor blood flow: Can cause pain and cramping, known as peripheral artery disease (PAD).
A comprehensive evaluation by a healthcare provider is often necessary to determine the precise reason of foot discomfort. A physical examination, a review of medical history, and diagnostic tests like MRIs or X-rays could all be part of this assessment..
HOW TO RELIEVE FOOT PAIN
Here are some specific treatments for common causes of foot pain:
Plantar Fasciitis
1. Stretching Exercises: Stretch your calves and the plantar fascia itself.
2. Night Splints: Wear a night splint to keep the foot in a dorsiflexed position.
3. Orthotics: Use arch supports or custom orthotic devices.
4. Physical Therapy: Specific exercises and treatments from a physical therapist.
Achilles Tendinitis
1. Rest and Ice: Rest your Achilles tendon and apply ice to reduce swelling.
2. Heel Lifts: Use heel lifts in shoes to reduce strain on the tendon.
3. Stretching and Strengthening: Perform calf stretches and strengthening exercises for the calf muscles.
4. Anti-inflammatory Medications: Use NSAIDs to reduce pain and inflammation.
Bunions
1. Proper Footwear: Wear shoes with a wide toe box and avoid high heels.
2. Padding: Use bunion pads to cushion the bunion.
3. Orthotics: Custom orthotic devices can help align the foot correctly.
4. Surgery: In severe cases, surgery might be required to correct the deformity
MetatarsalGia
1. Rest: Reduce activities that cause foot stress.
2. Ice: Apply ice packs to reduce swelling and pain.
3. Arch Supports: Use insoles to distribute pressure more evenly across the foot.
4. Proper Footwear: Wear shoes with shock-absorbing soles and a wide toe box.
Morton’s Neuroma
1. Footwear Changes: Wear shoes with a wider toe box and avoid high heels.
2. Padding: Use metatarsal pads to relieve pressure on the nerve.
3. Injections: Corticosteroid injections can reduce inflammation and pain.
4. Surgery: In persistent cases, surgery may be needed to remove the affected nerve.
General Tips for Foot Pain
Relieving foot pain can depend on the cause of the pain, but here are some general methods that might help:
1. Maintain a Healthy Weight: Reducing weight can lessen the stress on your feet.
2. Stay Active: Engage in low-impact exercises like swimming or cycling.
3. Foot Hygiene: Keep your feet clean and dry to prevent infections.
4. Regular Checkups: Regularly visit a podiatrist for foot health checkups.
5. Rest and Elevation: Resting your feet and elevating them can reduce swelling and alleviate pain.
6. Cold Compress: Applying a cold pack to the painful area for 15-20 minutes can reduce inflammation and numb the area.
7. Foot Soaks: Soaking your feet in warm water with Epsom salts can relax muscles and reduce pain.
8.Proper Footwear: Wearing supportive and properly fitting shoes can prevent and alleviate foot pain.
9.Stretching Exercises: Regular stretching of the feet and calves can improve flexibility and reduce pain, particularly for conditions like plantar fasciitis.
10. Orthotic Inserts: Custom or over-the-counter orthotic inserts can provide additional support and alleviate pressure on painful areas.
11.Massage: Gently massaging the foot can improve blood flow and reduce tension.
12. Pain Relief Medication: Over-the-counter pain relievers like IBUPROFEN or ACETAMINOPHEN can help reduce pain and inflammation.
13. Foot Exercises: Exercises like toe curls, picking up objects with your toes, and rolling a tennis ball under your foot can strengthen foot muscles and alleviate pain.
14. Consult a Professional: If foot pain persists, it’s important to consult a healthcare professional, such as a podiatrist, for a proper diagnosis and treatment plan.
Implementing these strategies can help manage and relieve foot pain effectively.
FAQs
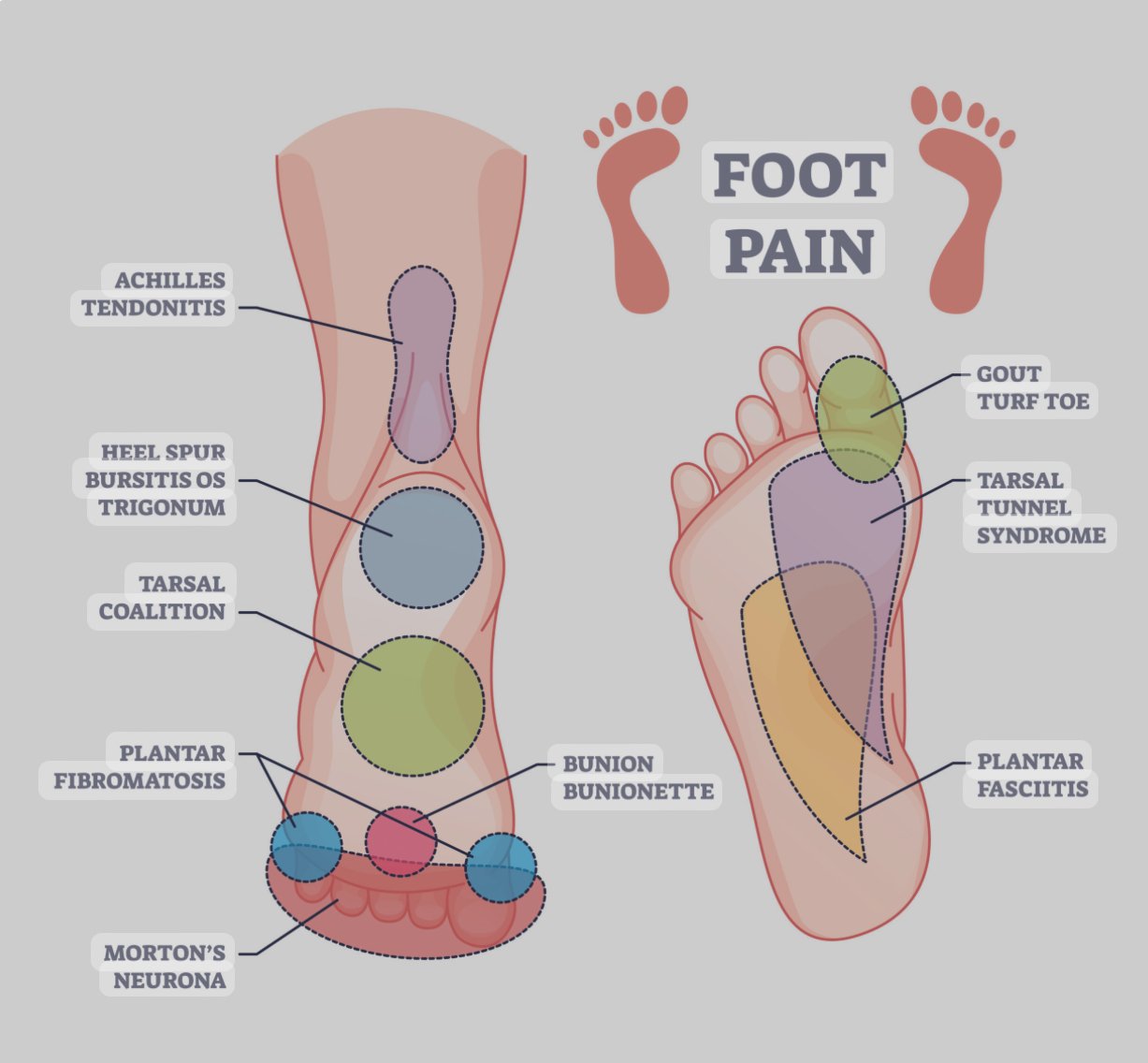
FOOT PAIN CHART
A foot pain chart is a diagram of the foot that helps identify and locate different types of pain and their possible causes. Here is a detailed foot pain chart with common areas of pain and their associated conditions:
Top of the Foot
– Pain Causes: Extensor Tendonitis, Stress Fractures, Gout, Bone Spurs
– Symptoms: Pain when lifting the foot, swelling, tenderness
Arch of the Foot
– Pain Causes: Plantar Fasciitis, Flat Feet, Arch Strain, Tarsal Tunnel Syndrome
– Symptoms: Sharp pain in the arch, especially in the morning or after standing
Heel
– Pain Causes: Plantar Fasciitis, Achilles Tendonitis, Heel Spurs, Bursitis
– Symptoms: Heel pain first thing in the morning, pain after standing or walking
Ball of the Foot
– Pain Causes: Metatarsalgia, Morton’s Neuroma, Sesamoiditis, Stress Fractures
– Symptoms: Sharp, aching pain in the ball of the foot, pain that worsens with activity
Toes
– Pain Causes: Bunions, Gout, Hammer Toe, Ingrown Toenail
– Symptoms: Swelling, redness, pain while walking, visible deformity
Outer Edge of the Foot
– Pain Causes: Peroneal Tendonitis, Cuboid Syndrome, Stress Fractures
– Symptoms: Pain along the outer edge of the foot, worsens with activity
Inner Edge of the Foot
– Pain Causes: Posterior Tibial Tendonitis, Bunions, Stress Fractures
– Symptoms: Pain along the inner edge, especially after standing or walking
Ankle
– Pain Causes: Sprains, Arthritis, Tendonitis, Fractures
– Symptoms: Swelling, bruising, pain during movement
How to Use This Chart?
1. Identify Pain Location: Pinpoint the area on the foot where the pain is most prominent.
2. Match Symptoms: Compare your symptoms with the common causes listed for that area.
3. Consult a Professional: For an accurate diagnosis and treatment plan, see a healthcare provider.
Finding the best treatment and avoiding more damage can be facilitated by being aware of the location of your foot discomfort and any potential reasons.
What is the best painkiller for foot pain?
The best painkiller for foot pain depends on the cause and severity of the pain, as well as individual health considerations. Here are the most commonly recommended options:
Over-the-Counter (OTC) Painkillers
1. Ibuprofen (Advil, Motrin)
– Uses: General pain relief and inflammation reduction.
– Pros: Effective for conditions involving inflammation, such as tendonitis or arthritis.
– Cons: Can cause stomach irritation with long-term use.
2. Naproxen (Aleve)
– Uses: Pain relief and inflammation reduction.
– Pros: Longer-lasting effects compared to ibuprofen.
– Cons: Similar risk of stomach irritation.
3. Acetaminophen (Tylenol)
– Uses: General pain relief.
– Pros: Gentle on the stomach, effective for mild to moderate pain.
– Cons: Does not reduce inflammation.
Prescription Painkillers
1. Stronger NSAIDs (e.g., Diclofenac)
– Uses: Severe pain and inflammation.
– Pros: Potent anti-inflammatory effects.
– Cons: Higher risk of side effects compared to OTC NSAIDs.
2. Opioids (e.g., Oxycodone, Hydrocodone)
– Uses: Severe pain, usually short-term use.
– Pros: Highly effective for intense pain.
– Cons: Risk of addiction, drowsiness, constipation.
Topical Pain Relievers
1. Diclofenac gel (Voltaren)
– Uses: Localized pain relief for arthritis and other conditions.
– Pros: Fewer systemic side effects, targeted relief.
– Cons: Possible skin irritation.
2. Capsaicin cream
– Uses: Localized pain relief, particularly for neuropathic pain.
– Pros: Effective for certain types of pain.
– Cons: Can cause burning sensation upon application.
When to Consult a Healthcare Provider
– Persistent Pain: If pain does not improve with OTC treatments.
– Severe Pain: If pain is intense and debilitating.
– Other Symptoms: If accompanied by swelling, redness, or fever.
– Chronic Conditions: For ongoing conditions like arthritis or plantar fasciitis, a tailored pain management plan may be necessary.
In the end, the finest painkiller will depend on specific conditions, therefore it’s better to speak with a healthcare professional to figure out the best course of action.
