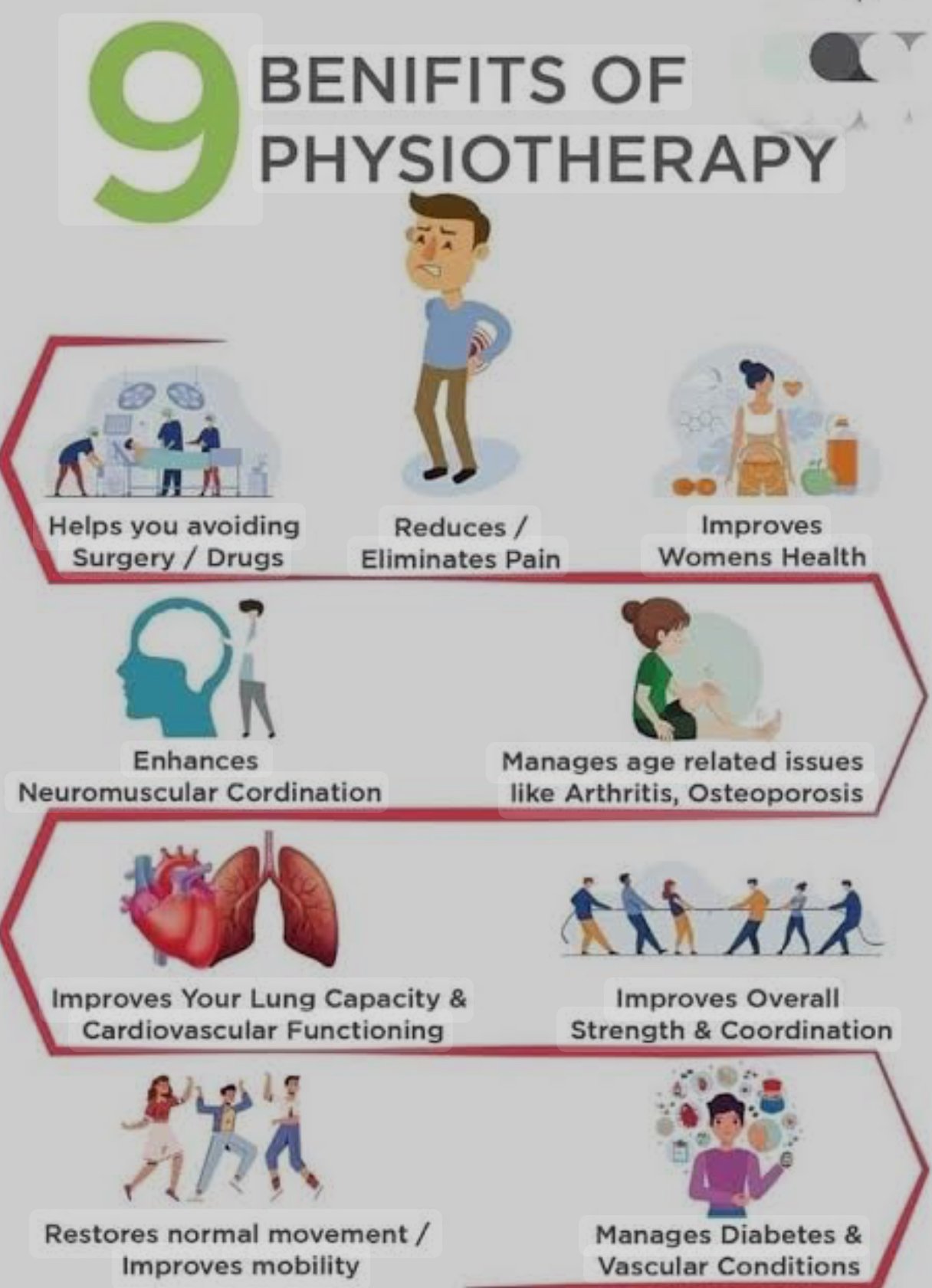
Can Physiotherapy Help In Diabetic Patients?
Indeed, physical treatment can be quite helpful in controlling diabetes and its side effects.. Diabetes, particularly Type 2 Diabetes, can lead to a range of musculoskeletal and neurological issues that affect movement and quality of life. Physiotherapy is useful in addressing these issues through a combination of exercise, education, and manual therapy. Here’s a detailed explanation of how physiotherapy can help diabetic patients:-

1.Improvement in Blood Sugar Control:-
.Role of Exercise:- Physical activity is a cornerstone of diabetes management. Regular exercise helps improve insulin sensitivity, allowing the body to use insulin more efficiently to lower blood sugar levels.
.Aerobic Exercise:- Activities like walking, swimming, or cycling can help in reducing blood sugar levels and improving cardiovascular health.
.Resistance Training:- Strengthening exercises increase muscle mass, which improves glucose uptake by muscles, aiding in better blood sugar control.
.Guided Exercise Programs:- Physiotherapists can create individualized exercise plans that consider a patient’s fitness level, comorbidities (like heart disease or neuropathy), and any physical limitation
.Understanding Neuropathy:- Diabetic neuropathy is a common complication where high blood sugar levels damage nerves, leading to symptoms like numbness, tingling, pain, or loss of sensation, particularly in the hands and feet. This may throw off balance, resulting in accidents or falls.
2.Management of Diabetic Neuropathy:-
Physiotherapy for Neuropathy:-
.Balance Training:- Exercises that improve balance and coordination can reduce the risk of falls. Physiotherapists may use techniques like standing on one leg, heel-to-toe walking, or using balance boards.
.Foot Care Education:- Since diabetic neuropathy often affects the feet, physiotherapists educate patients about proper foot care, including choosing appropriate footwear and performing regular foot checks to avoid ulcers or infections.
.Pain Management:- For those with neuropathic pain, physiotherapy techniques like transcutaneous electrical nerve stimulation (TENS), gentle massage, and stretching can help manage discomfort.
.Gait Training:- If neuropathy affects walking, physiotherapists can help retrain the patient to walk with proper mechanics, reducing the risk of injury.
3.Cardiovascular Health:-
Diabetic patients are at higher risk of developing cardiovascular diseases. Physiotherapists can HELP by suggesting exercise routines that are good for the HEART.
- Low-Impact Cardiovascular Exercises: Such as brisk walking, swimming, or cycling to enhance heart function and endurance.
- Monitoring and Education: Teaching patients to monitor their heart rate and blood pressure during exercise to prevent any adverse events.
4.Weight Management
Weight management is crucial for Type 2 diabetes patients. Dietary recommendations together with physiotherapy therapies can greatly aid in improving glycemic control and lowering body fat.
.Wait loss training:- High-intensity interval training, or HIIT, is a weight-loss strategy that alternates brief bursts of high-intensity exercise with low- or no-intensity activities.
Behavioral Modification:- Encouraging lifestyle changes, such as increasing daily activity levels, improving posture, and reducing sedentary behavior.
5.Education and Self-Management:-
Physiotherapists educate diabetic patients about the importance of physical activity, proper posture, ergonomics, and foot care.
Self-Monitoring:- Patients are taught how to check their blood sugar levels before and after exercise in order to prevent hypo- or hyperglycemia.
Foot Care Education:- Guidance on foot hygiene, selection of appropriate footwear, and recognition of early signs of diabetic foot ulcers.
6.Hydrotherapy and Aquatic Exercises:-
For patients with joint pain, obesity, or difficulty with land-based exercises, aquatic therapy can be a good alternative. The buoyancy of water reduces JOINT STRAIN while offering resistance for muscle training.
7.Postural and Gait Training:-
Diabetic patients may experience postural changes and altered gait patterns due to muscle weakness, joint problems, or neuropathy. Physiotherapists can help with postural alignment, gait re-training, and providing assistive devices if necessary
8.Risk factor in diabetic:- patient’s:-Diabetes increases the risk of certain musculoskeletal disorders,including frozen shoulder, carpal tunnel syndrome, trigger finger, and tendinopathyThese ailments may result in pain, stiffness, and decreased range of motion..
Specific Conditions Addressed by Physiotherapy:-
.Frozen Shoulder (Adhesive Capsulitis):- This condition is more common in diabetics and leads to stiffness and pain in the shoulder joint. To regain range of motion and lessen pain, physiotherapy treatments include stretching routines, joint mobilizations, and passive range-of-motion exercises.
.Tendinopathies:- Tendon inflammation (such as in the Achilles or rotator cuff) is common in diabetics. Physiotherapists use eccentric motions, ICE therapy, and ultrasound therapy to promote tendon repair.
.Carpal Tunnel Syndrome:- Caused by nerve compression in the wrist, leading to pain and numbness in the hands. Physiotherapists may use nerve gliding exercises, splinting, and manual therapy to relieve symptoms.
9.Use of Assistive Devices:-
- Orthotics:- Custom-made insoles to provide support and protection to diabetic patients with foot deformities or neuropathy.
- Walking Aids:- For patients with balance issues or weakness in the lower limbs, using canes or walkers can enhance mobility and prevent falls.
10.Breathing Exercises and Relaxation Techniques:-
Diabetes can also affect respiratory function due to poor cardiovascular health.Relaxation methods and breathing exercises, such diaphragmatic breathing, can be used to lower stress and increase oxygenation.
11. Monitoring and Preventing Complications:-
- Blood glucose:- monitoring:Physiotherapists need to ensure that patients are monitoring their blood glucose levels, especially before and after exercise, to avoid hypoglycemia caused by exercise.
- Blood Pressure Monitoring:-Before beginning any fitness regimen, blood pressure should be checked due to the elevated risk of cardiovascular disease.
Special Considerations:-
- Hypoglycemia Management:- Patients on insulin or oral hypoglycemic drugs may be at risk of low blood sugar during exercise. Education on signs of hypoglycemia and carrying fast-acting carbohydrates (e.g., glucose tablets) is important.
- Avoiding High-Impact Activities:- High-impact or strenuous activities should be avoided in patients with severe complications like advanced retinopathy or neuropathy.
- Progressive Exercise:- Exercise programs should start slow and gradually increase in intensity, especially in sedentary patients.
Summary:-
PHYSICAL ACTIVITIES, NEUROPATHY, MUSCULOSKELETAL PROBLEMS, CARDIOVASCULAR HEALTH, and patient education are all addressed in the holistic, TAILORED approach that is physiotherapy in the management of DIABETES. Physiotherapists create INDIVIDUALISED plans to help patients become more MOBILE, FEEL LESS PAIN, become STRONGER, and avoid complications from DIABETES, all of which improve QUALITY OF LIFE.